PROSTATE CANCER
Incidence:
200,000 American men per year
Death rate:
30,000 per year
Diagnosis:
Most men are diagnosed by an elevated prostate specific antigen blood test (PSA).
Less commonly, by an abnormal digital rectal examination (DRE)
PROSTATE SPECIFIC ANTIGEN (PSA)
A protein produced by the prostate
Measures the amount of PSA in a sample of blood
Most men with prostate cancer have an elevated PSA (greater than 4 ng/mL)
An elevated PSA level does not mean there is a cancer
The most common cause for an elevated PSA is benign prostatic hyperplasia (BPH), a noncancerous enlargement of the prostate.
Only 30 percent of men with an elevated PSA have prostate cancer.
PSA:
Less than 10 ng/mL is 70 to 80 percent have organ-confined disease
10 to 50 ng/L is 50 percent have organ-confined disease
Higher than 50 ng/ml is 25 percent organ confined
J Urol 1993; 150:110
PSA may not be elevated with Gleason score 8 and above
PROSTATE BIOPSY
Generally recommended if:
The prostate is enlarged or irregularly shaped on rectal examination
The following risk factors are present:
Age
All men are at risk for prostate cancer
Risk greatly increases with older age
Rarely found prostate in men younger than 50 years of age
Ethnic background —
Black men develop prostate cancer more often than white men
Black men are more likely to die of prostate cancer than white men.
Family medical history —
Men who have a first-degree relative (a father or brother) with prostate cancer are more likely to develop the disease
Elevated or increasing PSA level since the previous year
GLEASON GRADE
A pathological grade of prostate cancer aggressiveness (from 1 to 5) obtained from a pathology specimen
1.Well differentiated (almost normal), least aggressive
2.Rarely spreads
3.Seldom spreads
4.Often spreads
5.Poorly differentiated, most aggressive, usually spreads. PSA may be low.
GLEASON SCORE
Calculated by adding the grades of the two most common areas of abnormal growth
Low Score: 2 to 4-not a threat in the patients lifetime
Intermediate Score: 5 to 7-most common (90% of males with prostate cancer)
High Score: 8 to 10-almost always metastatic
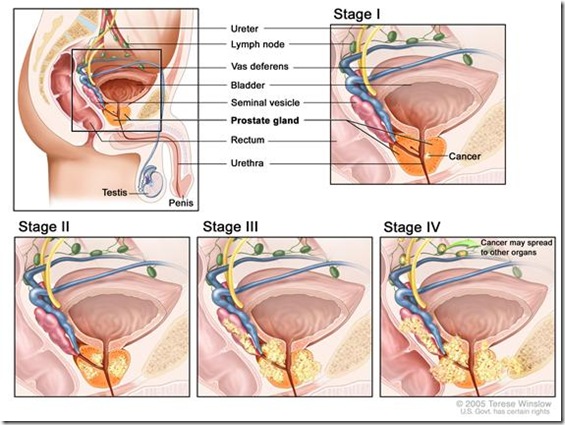
PROSTATE CANCER STAGE OR EXTENT OF DISEASE
Tumor-node-metastasis (TNM) system
Clinical staging determined by digital rectal examination(DRE)
Pathological staging determined by microscopic examination of tissue
CANCER STAGE
Tumor
Normal Anatomy
Images from the National Cancer Institute www.cancer.gov
T1 tumors are microscopic and cannot be felt during rectal examination
T2 tumors can be felt with a rectal examination, but appear to be confined to the prostate gland
T3 tumors have grown beyond the prostate into the capsule
T4 tumors have grown locally beyond the prostate, and involve nearby tissues
T3 or T4 tumor are not likely to be cured, even by surgery
Regional and Distant Lymph Nodes where prostate cancer is found
The regional lymph nodes are the nodes of the true pelvis, which are:
The pelvic nodes below the bifurcation of the common iliac arteries
They include the following groups:
Pelvic, not otherwise specified (NOS)
Hypogastric
Obturator
Iliac (internal, external, or NOS)
Sacral (lateral, presacral, promontory, or NOS)
Albertsen PC, Hanley JA, Harlan LC, et al. J Urol 2000;163:1138–1143
Distant lymph nodes where cancer of the prostate is found. These lie outside the confines of the true pelvis.
General diagram of lymph node areas
Distant lymph nodes include:
(Refer to the general diagram for the specific sites where prostate cancer may spread. These specific sites are are listed below)
Aortic (para-aortic lumbar)
Common iliac
Inguinal, deep and superficial (femoral)
Supraclavicular
Cervical
Scalen
Retroperitoneal, NOS
CA Cancer J Clin 2008; 58:54-59
Metastasis
Peripheral white area in the bone of the lower lumbar vertebrae and sacrum is prostate cancer. Metastatic lymph nodes of the pelvis surround the pelvic vessels
Osteoblastic metastases are the most common non-nodal site of prostate cancer metastasis (M1b)
Other non-bony sites would include:
Lung
Liver
Adrenal gland
Peritoneum or visceral sites (M1c)
Flanigan RC, McKay TC, Olson M, et al. Urology 1996;48:428–432
BONE SCAN
Recommended for men with high-grade Gleason scale
Not usually necessary with:
Low-grade (T1 or T2) cancer on physical examination
A Gleason score of less than or equal to 6
PSA value less than 10 ng/mL
CT (COMPUTED TOMOGRAPHY) SCAN OF THE ABDOMEN AND PELVIS
To determine the spread beyond the prostate
Not usually necessary:
With low-grade (T1 or T2) cancer on physical examination Gleason score of less than or equal to 6
PSA value less than 10 ng/mL
ENDORECTAL COIL MRI
Magnetic Resonance Imaging to assess the prostate and the surrounding tissues
Not in widespread use
PROS AND CONS OF SCREENING
Effectiveness of Prostate Cancer Screening:
Effective prostate cancer screening must:
Reduce disease-specific morbidity and/or mortality
Clinical trials
No benefit in morbidity and mortality has been found from current randomized, controlled screening trials
Cochrane Database Syst Rev. 2006 Jul19;3:CD004720
Results from two large trials will not be available for several years
JAMA 1995 Feb 15;273(7):548-52; Cancer 2004 Apr 1;100(7):1397-405; J Urol 2005 Aug;174(2):489-94; discussion 493-4
Evidence from observational studies:
There is a decline in:
Incidence of advanced stage disease
Mortality rates
SEER Cancer Statistics Review, 1973-1999. National Cancer Institute, Bethesda, MD, 2002
Harm from screening
<1 percent) cause complications serious enough to require hospitalization
Urology 1997 Jun;49(6):875-80
Anxiety and physical discomfort
J Natl Cancer Inst 1998 Jun 17;90(12):925-31
Discomfort with the procedure (55%)
Pain persisting longer than one week (2%)
Psychological distress even with a negative biopsy
Am J Med 2004 Nov 15;117(10):719-25; J Gen Intern Med. 2006 Jul;21(7):715- 21
Chronic anxiety after a negative prostate biopsy because:
Cancer cannot be ruled out
High false-negative biopsy rate
Urology 1997 Dec;50(6):831-2
Overdiagnosis
Screening-detected prostate cancers have early-stage disease and will be offered aggressive treatment.
Risk of overdiagnosis with screening found in:
29 percent of cancers detected in whites
44 percent of cancers detected in blacks
J Natl Cancer Inst 2002 Jul 3;94(13):981-90
50 percent overdetection in ages 55 to 67
J Natl Cancer Inst 2003 Jun 18;95(12):868-78
Outline adapted from UpToDate ® Eric A Klein, MD Section Editor
Last literature review version 16.1: January 2008
ASSESSMENT OF CURRENT PROSTATE SCREENING PROGRAMS
It can be concluded from the above discussion that optimal screening for prostate cancer has not yet been achieved.
The greatest advantage from current screening is in raising an awareness of the need for early detection, while cancer is still confined within the prostate gland , a time when it can be successfully removed by surgery.
The current system does not screen for the preconditions that lead to malignant degeneration in the first place. All the current system does is to identify prostate cancer after it has developed. Once malignant transformation has occurred, treatment is much more difficult.
There is a need for a system of screening that can detect the preconditions that lead to the formation of cancer and one that can identify those conditions that prevent tumor resolution.
I believe that a system of electrodermal detection and signal modulation can be developed to address these concerns. I hope to present an evidence based non-invasive, cost effective method of electrodermal screening and treatment of prostate cancer in my future discussions.
Vincent J. Speckhart MD MD(H)